Robots can’t care — and believing they can will break our health system

Matthew Kayne
- Published
- Opinion & Analysis

Artificial intelligence is being hailed as the next frontier in healthcare but as broadcaster and disability rights advocate Matthew Kayne writes, empathy cannot be automated. Real care exists in human presence, in the moments of understanding that only people can offer
We live in an age where technology promises to fix everything — from hospital waiting lists to loneliness. Artificial intelligence is now being tested to monitor patients, predict illness, and even provide “companionship.” But as someone who has lived through the human reality of care systems, I can’t help asking: Can a machine ever truly care?
Technology can do many remarkable things. It can track your heartbeat, remind you to take medication, or alert doctors in emergencies. But care is not just about process — it’s about presence. It’s the hand that reassures you when you’re scared, the voice that listens when you feel invisible, the connection that reminds you that you still matter. No algorithm, however advanced, can replicate that.
I’ve spent years navigating health and social care systems that often forget that simple truth. I’ve seen what happens when bureaucracy replaces empathy — when decisions are made based on cost instead of compassion. Now, as AI becomes the next big solution, I fear we risk making the same mistake all over again, just with shinier tools.
The problem isn’t technology itself. In fact, innovation could transform the lives of disabled people if used responsibly. Smart homes, adaptive devices, and digital assistants have already made independence possible for many who were once trapped by barriers. But what worries me is when we start believing that empathy can be automated — that emotional understanding can be outsourced to software.
During my battle with bladder cancer, I learned that care is an art as much as a science. The best doctors weren’t necessarily the ones with the fanciest machines; they were the ones who looked me in the eye and saw me as a person, not a patient. They made me feel human again. That’s something no line of code can achieve.
The truth is, people don’t just need treatment — they need to be heard. Yet, as funding pressures grow and workloads rise, some leaders see AI as a way to fill emotional gaps in care. There are now “AI companions” being marketed to care homes, promising to keep residents company. But is that company — or just digital loneliness disguised as help?
When care becomes mechanical, people become invisible. The risk isn’t that AI will take over — it’s that it will make us forget what makes us human.
The irony is that empathy is what we most need and what we most overlook. When I fought for my right to independence and for better wheelchair services, the biggest problem wasn’t lack of policy — it was lack of listening. Decisions were made about my life without me in the room. It’s the same principle at play with technology: progress that happens to people, not with them.
I believe AI can be a force for good — but only if it’s guided by people who understand care on a human level. What we need is ethical innovation, not just efficiency. Every new system should start with one question: Does this make someone’s life more human, or less?
That’s where lived experience must lead the way. Policymakers and developers need to listen to those of us who know what it’s like to depend on care — not just as test cases, but as co-creators. Disabled people, older people, and those with long-term conditions should be sitting at the design table, shaping how technology supports dignity and autonomy.
There’s huge potential in AI for accessibility — imagine software that helps people communicate, or predictive tools that prevent crises before they happen. But these innovations must never replace the heart of care. Technology should empower compassion, not erase it.
The danger is not that robots will replace nurses — it’s that we start treating nurses like robots, pressured to perform tasks faster and cheaper at the expense of empathy. Once we start measuring care in metrics instead of moments, we’ve already lost something sacred.
When I wrote my song Free Like a Bird, it was about that same feeling — the tension between control and freedom. Between being monitored and being understood. Technology can set us free, but only if it serves the person, not the system.
We stand at a crossroads. We can build a future where AI enhances care — or one where it empties it of feeling. The difference will depend on one thing: whether we still believe that empathy matters.
As we embrace the machines, let’s not forget the miracle of being human.

Matthew Kayne is broadcaster, political campaigner and disability rights advocate who has turned personal challenges into platforms for change. He is the founder and owner of Sugar Kayne Radio, an online station dedicated to uplifting music and meaningful conversations, and the leader of a national petition calling for reform of the UK’s wheelchair service. Living with cerebral palsy and a survivor of bladder cancer, Matthew channels his lived experience into advocacy, broadcasting, and songwriting. His long-term ambition is to bring this experience into politics as an MP, championing disability rights, healthcare access, and workplace inclusion.
READ MORE: ‘Why NHS cancer care still fails disabled people‘. Matthew Kayne has lived through the best and worst of Britain’s healthcare system. Diagnosed with bladder cancer and living with cerebral palsy, he saw first-hand how poor communication, slow services and systemic indifference make recovery harder for disabled patients — and why urgent reform is long overdue.
Do you have news to share or expertise to contribute? The European welcomes insights from business leaders and sector specialists. Get in touch with our editorial team to find out more.
Main image: Pavel Danilyuk/Pexels
RECENT ARTICLES
-
 The era of easy markets is ending — here are the risks investors can no longer ignore
The era of easy markets is ending — here are the risks investors can no longer ignore -
 Is testosterone the new performance hack for executives?
Is testosterone the new performance hack for executives? -
 Can we regulate reality? AI, sovereignty and the battle over what counts as real
Can we regulate reality? AI, sovereignty and the battle over what counts as real -
 NATO gears up for conflict as transatlantic strains grow
NATO gears up for conflict as transatlantic strains grow -
 Facial recognition is leaving the US border — and we should be concerned
Facial recognition is leaving the US border — and we should be concerned -
 Wheelchair design is stuck in the past — and disabled people are paying the price
Wheelchair design is stuck in the past — and disabled people are paying the price -
 Why Europe still needs America
Why Europe still needs America -
 Why Europe’s finance apps must start borrowing from each other’s playbooks
Why Europe’s finance apps must start borrowing from each other’s playbooks -
 Why universities must set clear rules for AI use before trust in academia erodes
Why universities must set clear rules for AI use before trust in academia erodes -
 The lucky leader: six lessons on why fortune favours some and fails others
The lucky leader: six lessons on why fortune favours some and fails others -
 Reckon AI has cracked thinking? Think again
Reckon AI has cracked thinking? Think again -
 The new 10 year National Cancer Plan: fewer measures, more heart?
The new 10 year National Cancer Plan: fewer measures, more heart? -
 The Reese Witherspoon effect: how celebrity book clubs are rewriting the rules of publishing
The Reese Witherspoon effect: how celebrity book clubs are rewriting the rules of publishing -
 The legality of tax planning in an age of moral outrage
The legality of tax planning in an age of moral outrage -
 The limits of good intentions in public policy
The limits of good intentions in public policy -
 Are favouritism and fear holding back Germany’s rearmament?
Are favouritism and fear holding back Germany’s rearmament? -
 What bestseller lists really tell us — and why they shouldn’t be the only measure of a book’s worth
What bestseller lists really tell us — and why they shouldn’t be the only measure of a book’s worth -
 Why mere survival is no longer enough for children with brain tumours
Why mere survival is no longer enough for children with brain tumours -
 What Germany’s Energiewende teaches Europe about power, risk and reality
What Germany’s Energiewende teaches Europe about power, risk and reality -
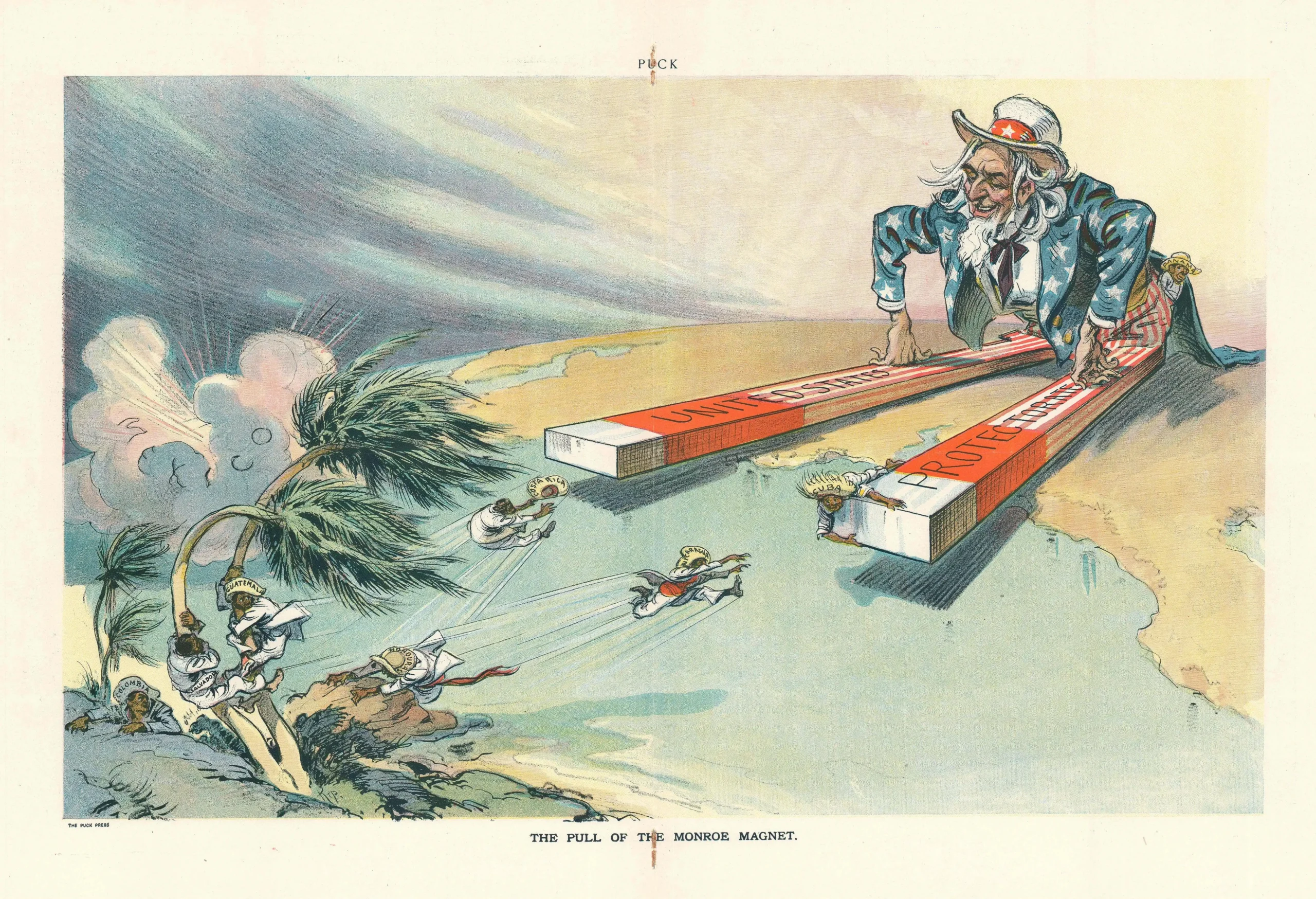
 What the Monroe Doctrine actually said — and why Trump is invoking it now
What the Monroe Doctrine actually said — and why Trump is invoking it now -
 Love with responsibility: rethinking supply chains this Valentine’s Day
Love with responsibility: rethinking supply chains this Valentine’s Day -
 Why the India–EU trade deal matters far beyond diplomacy
Why the India–EU trade deal matters far beyond diplomacy -
 Why the countryside is far safer than we think - and why apex predators belong in it
Why the countryside is far safer than we think - and why apex predators belong in it -
 What if he falls?
What if he falls? -
 Trump reminds Davos that talk still runs the world
Trump reminds Davos that talk still runs the world