Do women face diagnostic delays in cancer?

Dr Mohammad Muneeb Khan
- Published
- Opinion & Analysis

Research shows that women often face longer waits for a cancer diagnosis than men. These delays are measured in lives, outcomes and lost opportunities for treatment. Here, our health and science correspondent Dr Mohammad Muneeb Khan examines the evidence, the causes and the urgent need for change, and asks whether bias, barriers and systemic blind spots are costing women their futures. His previous article, Trust Me, I’m a Doctor: Here’s How to Spot Cancer Misinformation Online, explores how misleading content can further harm patients and delay care
When the shadow of illness falls, the time spent waiting for a diagnosis can cost more than the disease itself. Recent research, together with the work of global charities such as Killing Cancer Kindly (KCK), has sharpened the focus on a pressing question: do women face longer delays in receiving a cancer diagnosis than men? The answer is both nuanced and urgent.
Global studies increasingly point to a troubling truth: across a range of conditions, women often wait longer for diagnosis. One wide-ranging analysis reported by Reuters found that women were diagnosed with diseases, including cancer, an average of 2.5 years later than men, with delays stretching to as much as 4.5 years for certain metabolic disorders. While not all cancers were specified, the pattern is consistent.
More targeted data from Spain shows that women with rectal cancer experienced significantly longer delays before diagnosis — 23.8% waited more than three months, compared with 15.7% of men, according to BMC Cancer. A further analysis of nearly 200,000 patients, published on arXiv, revealed that women consistently faced longer “time-to-diagnosis” intervals regardless of how their disease presented. These numbers are not abstract: they represent days and weeks in which treatment could have begun, disease stages might have shifted, and outcomes could have improved.
The reasons for this disparity are complex. In clinics, symptoms that should trigger alarm are too often reassured away. Chest pain becomes indigestion; weight loss is written off as stress.
When women present vague or diffuse symptoms, clinicians may attribute them to psychological or benign causes instead of investigating further. This tendency is well documented among racial and ethnic minorities and appears with equal force in gender bias within cancer care. In many parts of the world, structural and social barriers compound the problem.
Cultural norms may delay women’s decision to seek medical advice, while mobility restrictions, caregiving responsibilities, or economic dependence can limit access to clinics and diagnostics. Stigma and fear — particularly around cancers of the breasts or reproductive organs — keep some women silent.
There are also disease-specific blind spots. In bladder cancer, for example, women are twice as likely as men to be treated for urinary tract infections before cancer is even considered, delaying accurate diagnosis by an average of 85 days compared with 74 days for men, according to Time. The phenomenon recalls the so-called “Yentl Syndrome” in cardiology, where women whose symptoms fall outside the traditional, male-oriented textbook descriptions see their conditions misinterpreted or dismissed entirely. Though not directly linked to cancer, it illustrates a systemic bias: when women do not fit the expected clinical pattern, the diagnosis is more likely to be missed.
The cost of delay is measured in lives and futures. Every day lost to misdiagnosis or slow referral reduces the range of treatment options, increases the likelihood of more aggressive interventions, and can turn a curable condition into one that is only manageable through palliative care.
Myths and misinformation add further harm, whether by encouraging women to pursue unproven remedies or by deterring them from screening altogether through shame, scarcity of resources, or adherence to tradition. In hospitals and community clinics, these realities are not theoretical. Families are left to grieve earlier than they might have had the diagnosis come even a month sooner.
Addressing this inequity requires a shift on several fronts. Clinicians need training that challenges assumptions about symptom patterns and reinforces gender-aware diagnostic vigilance. Community screening programmes must be supported, particularly in low- and middle-income regions where barriers are most acute.
Women should be equipped with accessible health literacy tools — from symptom checklists and guidance on when to seek help, to encouragement for obtaining second opinions. Public and social media can also play a role, portraying women who speak up early, confront stigma, and demand timely care.
Diagnostic time is precious. It should be determined by medical need rather than by chance or bias. If women are reaching the clinic later, the responsibility lies with policy, practice, and trust to bring them in sooner. For every delay that tips the scales of equity, swift recognition is the counterbalance that can change the course of a life.

Dr Mohammad Muneeb Khan (M.B.B.S, M.R.C.P, MSc, F.R.C.R) is a leading expert in cancer prevention and the founder of Killing Cancer Kindly, a UK-based international cancer awareness charity. With over 25 years of clinical and research experience, he has served as principal investigator on numerous national and international cancer trials and is a passionate advocate for cancer prevention, evidence-based treatment, and public education.
Dr Khan is also the author of You’ll Wish You Were an Elephant: Killing Cancer Kindly and The How, What & Why of Cancer: Separating Fact from Fiction.
Main photo: Thirdman/Pexels
RECENT ARTICLES
-
 Why Europe still needs America
Why Europe still needs America -
 Why Europe’s finance apps must start borrowing from each other’s playbooks
Why Europe’s finance apps must start borrowing from each other’s playbooks -
 Why universities must set clear rules for AI use before trust in academia erodes
Why universities must set clear rules for AI use before trust in academia erodes -
 The lucky leader: six lessons on why fortune favours some and fails others
The lucky leader: six lessons on why fortune favours some and fails others -
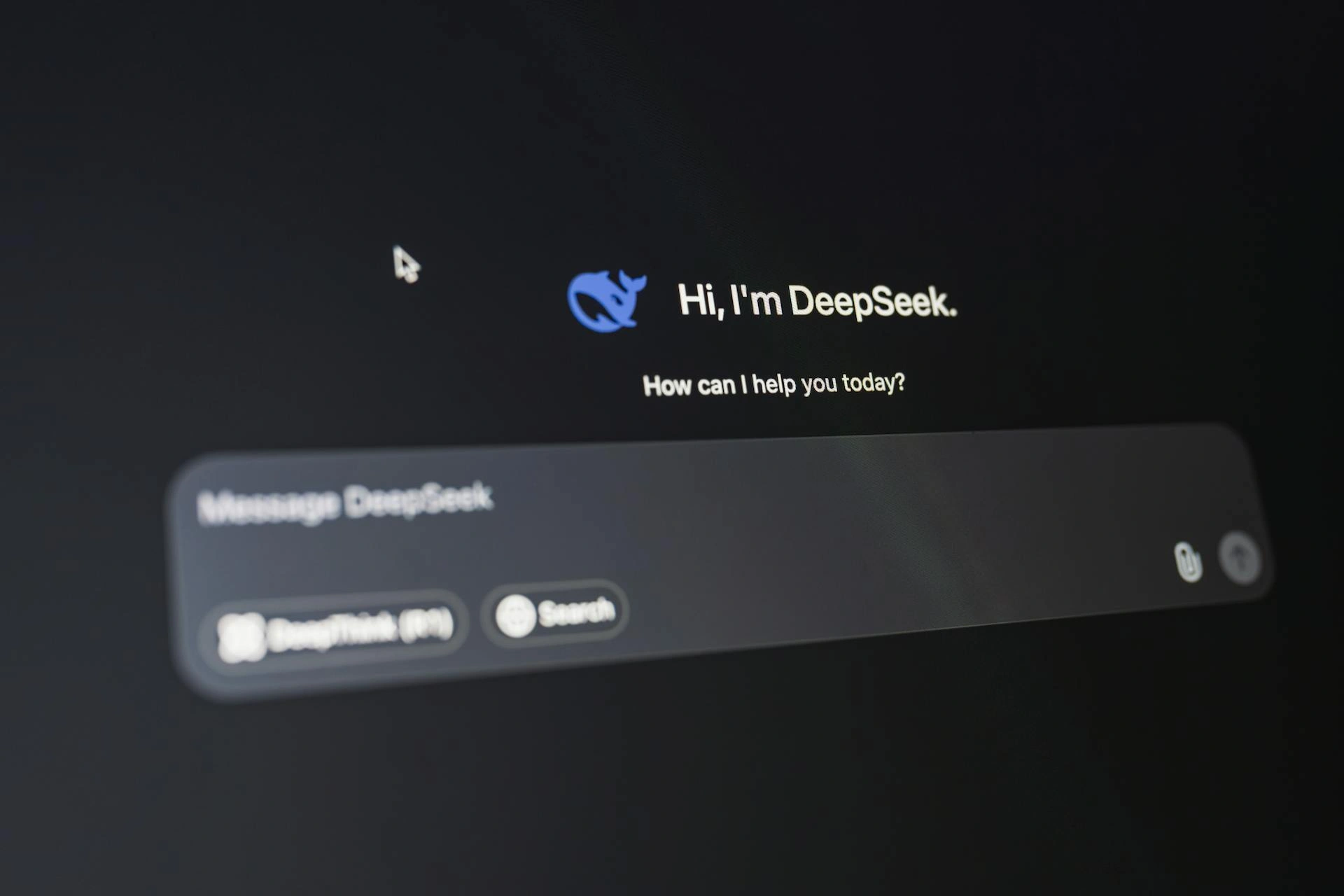
 Reckon AI has cracked thinking? Think again
Reckon AI has cracked thinking? Think again -
 The new 10 year National Cancer Plan: fewer measures, more heart?
The new 10 year National Cancer Plan: fewer measures, more heart? -
 The Reese Witherspoon effect: how celebrity book clubs are rewriting the rules of publishing
The Reese Witherspoon effect: how celebrity book clubs are rewriting the rules of publishing -
 The legality of tax planning in an age of moral outrage
The legality of tax planning in an age of moral outrage -
 The limits of good intentions in public policy
The limits of good intentions in public policy -
 Are favouritism and fear holding back Germany’s rearmament?
Are favouritism and fear holding back Germany’s rearmament? -
 What bestseller lists really tell us — and why they shouldn’t be the only measure of a book’s worth
What bestseller lists really tell us — and why they shouldn’t be the only measure of a book’s worth -
 Why mere survival is no longer enough for children with brain tumours
Why mere survival is no longer enough for children with brain tumours -
 What Germany’s Energiewende teaches Europe about power, risk and reality
What Germany’s Energiewende teaches Europe about power, risk and reality -
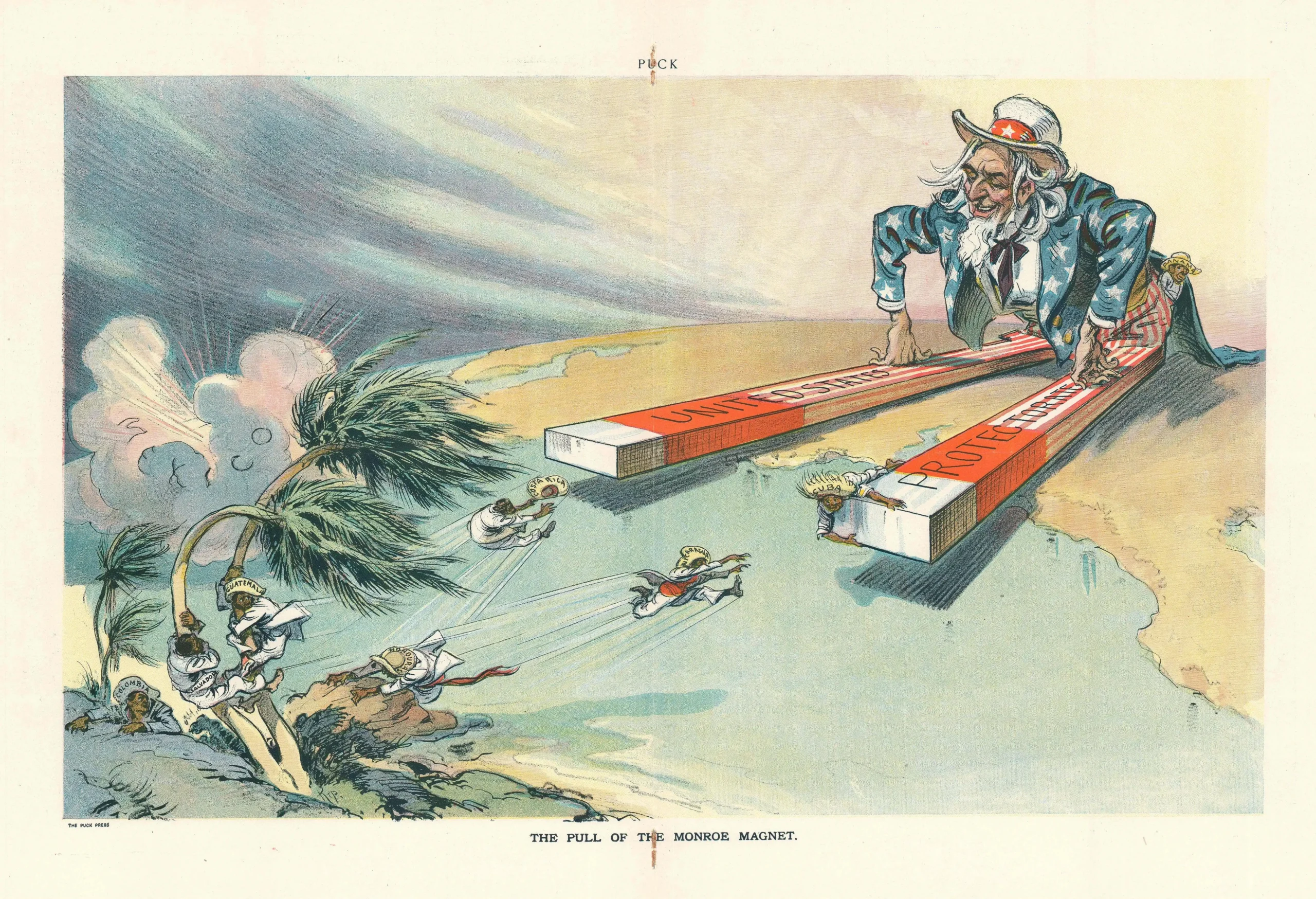
 What the Monroe Doctrine actually said — and why Trump is invoking it now
What the Monroe Doctrine actually said — and why Trump is invoking it now -
 Love with responsibility: rethinking supply chains this Valentine’s Day
Love with responsibility: rethinking supply chains this Valentine’s Day -
 Why the India–EU trade deal matters far beyond diplomacy
Why the India–EU trade deal matters far beyond diplomacy -
 Why the countryside is far safer than we think - and why apex predators belong in it
Why the countryside is far safer than we think - and why apex predators belong in it -
 What if he falls?
What if he falls? -
 Trump reminds Davos that talk still runs the world
Trump reminds Davos that talk still runs the world -
 Will Trump’s Davos speech still destroy NATO?
Will Trump’s Davos speech still destroy NATO? -
 Philosophers cautioned against formalising human intuition. AI is trying to do exactly that
Philosophers cautioned against formalising human intuition. AI is trying to do exactly that -
 Life’s lottery and the economics of poverty
Life’s lottery and the economics of poverty -
 On a wing and a prayer: the reality of medical repatriation
On a wing and a prayer: the reality of medical repatriation -
 Ai&E: the chatbot ‘GP’ has arrived — and it operates outside the law
Ai&E: the chatbot ‘GP’ has arrived — and it operates outside the law -
 Keir Starmer, Wes Streeting and the Government’s silence: disabled people are still waiting
Keir Starmer, Wes Streeting and the Government’s silence: disabled people are still waiting