How AI and supercomputers could revolutionise personalised medicine

Professor Syma Khalid
- Published
- Opinion & Analysis

The combination of artificial intelligence, advanced molecular modelling and genomic sequencing could transform medicine. With the right investment, the UK could lead this change, writes Professor Syma Khalid of the University of Oxford
Artificial Intelligence is advancing into every area of life. Recently, two potential drugs – one against gonorrhoea, another against MRSA – were designed entirely by AI. In parallel, the UK government has announced significant funding for a new national supercomputer and wider AI research, part of its plan to secure Britain’s position in global technology.
It is not hard to picture what this could mean for medicine. Imagine the year is 2040 and you are diagnosed with a disease that would prove fatal today. Within 24 hours, a laboratory has analysed molecules from your body and produced a drug precisely tailored to you. This may sound ambitious, but the government’s planned investment in computing infrastructure could make such a future possible.
To understand the link between computing and drug development, it helps to look at how many medicines are created today. For more than thirty years, chemists have used computer simulations based on the laws of physics to model the behaviour of molecules in the body. These simulations provide insights into how biological systems work and how they can be altered to treat disease. In my own case, the appeal of this field – known as computational chemistry – came from being able to combine a long-standing interest in computers and video games with chemistry, using computer graphics to create moving images of molecules interacting in real time.
Even now, watching a simulated protein move and unexpectedly expose a possible drug target is an incredible, exciting experience. These techniques have been used in the discovery of at least 70 approved drugs, including Novartis’s cancer treatment Gleevec and Roche’s influenza drug Tamiflu. Early work in this field often stayed within the walls of the researcher’s own institution, but as computers have become more powerful, the simulations have grown in accuracy and predictive power.
However, most simulations are still simplified. They often resemble a chemist’s test tube, containing water, the intended target and the drug. This approach cannot account for the full complexity of human biology and is unable to predict side-effects or differences in how people respond to the same treatment. To overcome this, we need models that more closely replicate living systems – that is, models which include the crowded, varied environments of cells, tissues and whole organisms.
This is where AI comes into its own. Complex models produce huge volumes of data that cannot easily be analysed by conventional computing or by human inspection. My team’s recent work on bacterial membranes, for example, showed that more complex models generate results in which trends are not obvious, even to experienced scientists. AI can process large datasets, identify patterns, and make predictions that guide further research.
Researchers have already begun combining AI with physics-based simulations. During the Covid-19 pandemic, this approach was used to predict the structure of the SARS-CoV-2 virus’s surface, a contribution recognised with the inaugural Gordon Bell Prize for Covid research.
The next logical step is to combine AI, advanced simulations and the fastest supercomputers to design drugs tailored to the biology of each individual. To do this, we must also understand the genetic differences between people. A familiar example is a bacterial infection treated in primary care: it can take more than one course of antibiotics to find one that works, even though all the drugs are effective in the laboratory. The reason is that genetic differences – which proteins are present in the body and in what amounts – affect how we respond to specific treatments. These variations are only now being mapped at scale.
Modern DNA sequencing technologies, such as those developed by Oxford Nanopore Technologies, are making it faster and cheaper to identify these differences. In one episode of our Science of the Times podcast, Gordon Sanghera, CEO of Oxford Nanopore Technologies, explained that our genomes contain information on our disease risks and how likely we are to benefit from particular drugs. Their sequencing techniques can uncover this information rapidly and economically. Integrating such genomic data into AI-driven simulations will be essential for creating truly personalised medicines.
This will require major infrastructure. Both AI and physics-based modelling need not only powerful processors but also high-capacity data storage, fast connections and skilled staff. The cost is high: the El Capitan and Frontier supercomputers in the United States each cost about $600 million, while Jupiter, installed in Jülich, Germany, cost about $500 million. Against this background, the UK government’s pledge of £1 billion for AI and £750 million for a new national supercomputer after the latest spending review is welcome, but must be seen as the first step in a sustained programme of investment.
Professor Jonathan Essex of the University of Southampton has noted that such facilities will enable the rapid development of new tools for drug design, particularly in antibody therapies: “We will be able to develop and apply new tools to design better pharmaceuticals much more quickly than before, particularly in the fast-changing area of antibody therapies.” But without long-term funding and strategic planning, the UK risks falling behind countries that have already made large, ongoing investments in this area.
For me, computational chemistry has always been about the combination of scientific rigour and technical innovation. I now feel a certain envy of my students and research team: this is an unprecedentedly exciting time to be working in the field. I still find it remarkable to watch a simulation reveal an unexpected possibility for treatment.
But the real goal is to ensure that when a patient is diagnosed, the right drug can be created for them without delay. If the UK builds the infrastructure and expertise now, those medicines could be developed here by scientists we have trained – perhaps even by me, or someone from my lab, when I reach old age and need them. If we do not, they will be developed elsewhere, and both the capability and the benefits will be lost.

Professor Syma Khalid is Professor of Computational Microbiology in the Department of Biochemistry at the University of Oxford, and a Fellow and Tutor at St Anne’s College. Her research specialising in the use of computer simulations to study the molecular machinery of microbes and its role in health and disease. She is the chair of HECBioSim which allocates resource on national and regional supercomputing facilities for biomolecular simulations. She is also cohost of the popular science podcast, Science of the Times
Main image: Google DeepMind
RECENT ARTICLES
-
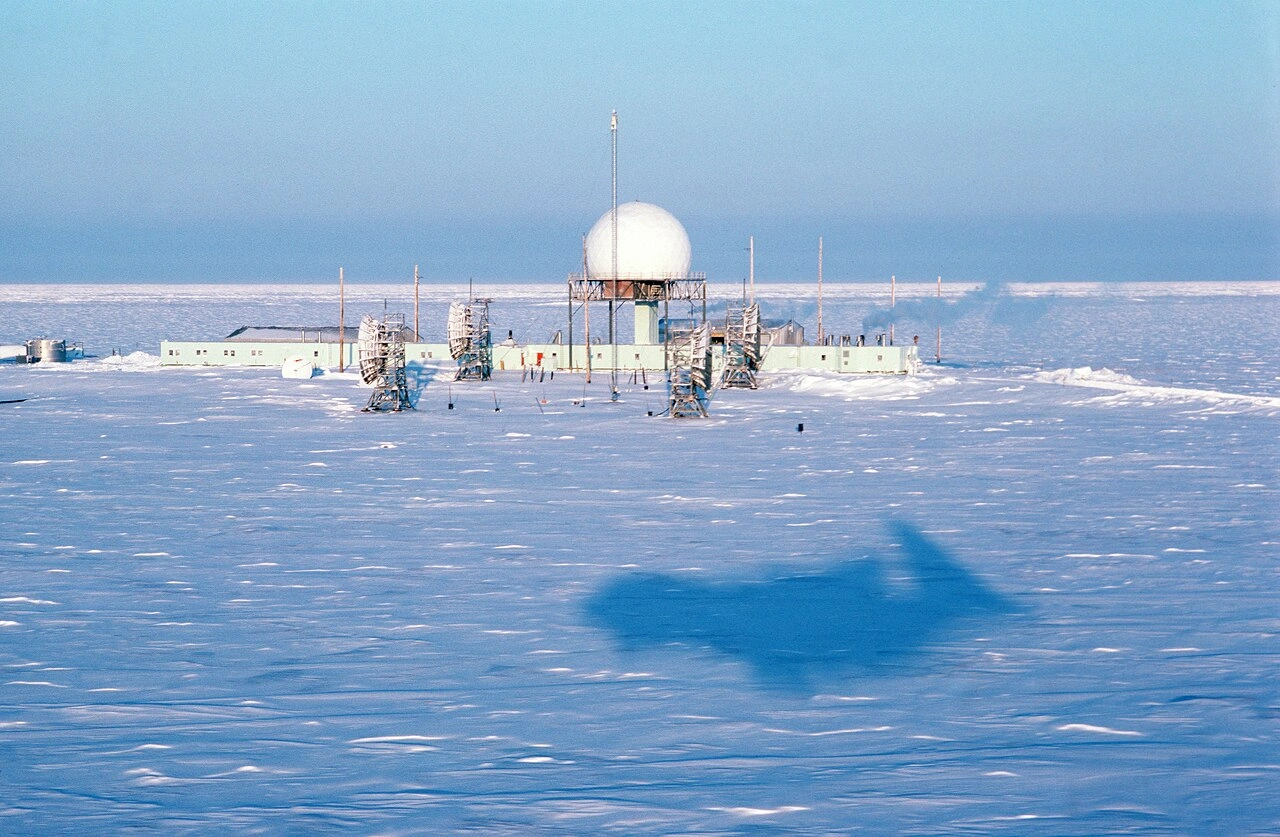
 The Arctic’s unfinished cold war
The Arctic’s unfinished cold war -
 Highway robbery: how the UK’s post-Brexit electric car policy blew a fuse
Highway robbery: how the UK’s post-Brexit electric car policy blew a fuse -
 Nokia built the brains for the AI network revolution — so why is American capital leading the charge?
Nokia built the brains for the AI network revolution — so why is American capital leading the charge? -
 What the UK SEND reform whitepaper means and what it might take to deliver it
What the UK SEND reform whitepaper means and what it might take to deliver it -
 Europe cannot call itself ‘equal’ while disabled citizens are still fighting for access
Europe cannot call itself ‘equal’ while disabled citizens are still fighting for access -
 Is Europe regulating the future or forgetting to build it? The hidden flaw in digital sovereignty
Is Europe regulating the future or forgetting to build it? The hidden flaw in digital sovereignty -
 The era of easy markets is ending — here are the risks investors can no longer ignore
The era of easy markets is ending — here are the risks investors can no longer ignore -
 Is testosterone the new performance hack for executives?
Is testosterone the new performance hack for executives? -
 Can we regulate reality? AI, sovereignty and the battle over what counts as real
Can we regulate reality? AI, sovereignty and the battle over what counts as real -
 NATO gears up for conflict as transatlantic strains grow
NATO gears up for conflict as transatlantic strains grow -
 Facial recognition is leaving the US border — and we should be concerned
Facial recognition is leaving the US border — and we should be concerned -
 Wheelchair design is stuck in the past — and disabled people are paying the price
Wheelchair design is stuck in the past — and disabled people are paying the price -
 Why Europe still needs America
Why Europe still needs America -
 Why Europe’s finance apps must start borrowing from each other’s playbooks
Why Europe’s finance apps must start borrowing from each other’s playbooks -
 Why universities must set clear rules for AI use before trust in academia erodes
Why universities must set clear rules for AI use before trust in academia erodes -
 The lucky leader: six lessons on why fortune favours some and fails others
The lucky leader: six lessons on why fortune favours some and fails others -
 Reckon AI has cracked thinking? Think again
Reckon AI has cracked thinking? Think again -
 The new 10 year National Cancer Plan: fewer measures, more heart?
The new 10 year National Cancer Plan: fewer measures, more heart? -
 The Reese Witherspoon effect: how celebrity book clubs are rewriting the rules of publishing
The Reese Witherspoon effect: how celebrity book clubs are rewriting the rules of publishing -
 The legality of tax planning in an age of moral outrage
The legality of tax planning in an age of moral outrage -
 The limits of good intentions in public policy
The limits of good intentions in public policy -
 Are favouritism and fear holding back Germany’s rearmament?
Are favouritism and fear holding back Germany’s rearmament? -
 What bestseller lists really tell us — and why they shouldn’t be the only measure of a book’s worth
What bestseller lists really tell us — and why they shouldn’t be the only measure of a book’s worth -
 Why mere survival is no longer enough for children with brain tumours
Why mere survival is no longer enough for children with brain tumours -
 What Germany’s Energiewende teaches Europe about power, risk and reality
What Germany’s Energiewende teaches Europe about power, risk and reality